Chronic Kidney Disease (CKD) is a condition characterized by a gradual loss of kidney function over time. Our kidneys play a crucial role in filtering waste and excess fluids from our blood, which are then expelled in our urine. As CKD progresses, it gradually leads to the buildup of toxic waste products in the body, which eventually causes serious health issues. At Northlake Nephrology Institute, we specialize in managing the course of Chronic Kidney Disease so that its progression is halted or at least slowed to the greatest degree. This approach gives our patients the highest quality of life for the longest time possible.
The CKD Prognosis Consortium offers several evidence-based tools for predicting progression of CKD based on several risk factors. Managing these risk factors is the cornerstone of effective CKD treatment.
Chronic Kidney Disease Management
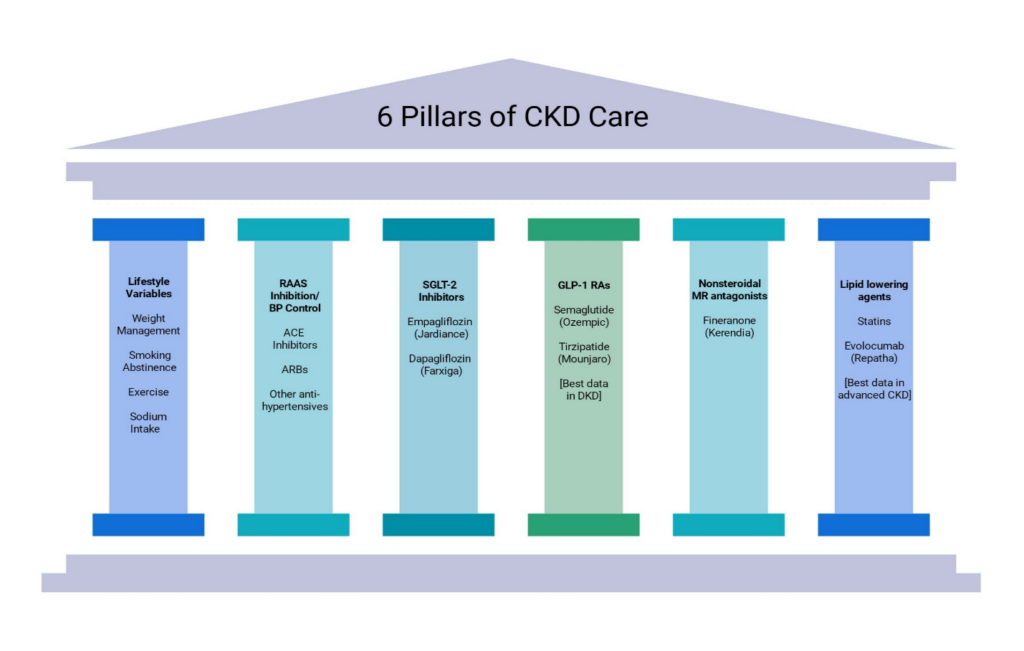
Chronic Kidney Disease management should be tailored specifically to each patient’s underlying kidney disease process, their other medical conditions, and their lifestyle. At Northlake Nephrology Institute, treatments may include lifestyle changes, such as diet, exercise, and sleep, as well as disease-modifying medications which preserve and protect kidney function. For more advanced cases, plans may include discussion for renal replacement such as kidney transplant or dialysis treatment options. Through every phase of treatment, our goal is always to halt the progression of CKD, alleviate symptoms, and enhance your quality of your life.
As discussed in more detail below, some specific causes of CKD require specific treatments; however, the progression of all types of CKD respond (to varying degrees) to the foundational treatments described here.
Of the treatments listed below, some have stronger evidence supporting their use and some have stronger treatment effects than others, depending on patient groups studied. In addition, based in part on the risk-of-progression models discussed above, a logical approach would be to treat patients with a more guarded prognosis more aggressively.
However, adding medications with little added benefit to low-risk patients is certainly not ideal. Each added medicine increases the risk of interaction with other medicines and increases the risk of adverse reactions. Your NNI provider will assess your individual risk and discuss these treatment options with you, and together map out an ideal treatment strategy.
- CKD – Chronic kidney Disease
- DKD – Diabetic Kidney Disease
- RAAS – Renin-Angiotensin-Aldosterone System
- ACE – Angiotensin Converting Enzyme
- ARB – Angiotensin Receptor Blocker
- SGLT-2 – Sodium Glucose Cotransporter-2
- GLP-1 RA – Glucagon-like Peptide-Receptor Agonist
- MR – Mineralocorticoid Receptor
Diabetic Kidney Disease
As with many forms of CKD, diabetes-related kidney disease usually begins with glomerular damage and leakage of proteins, particularly albumin, into the urine. Over time, the protein spillage increases and gradually kidney function declines. What sets diabetes-related kidney disease, or diabetic nephropathy (DN), apart from other common causes of CKD is the rate of decline in kidney function, which is generally more rapid than with other etiologies. Because of the more rapid progression of disease, early use of medical interventions often has dramatic positive effects. And the early introduction of these medicines is crucial to halting or mitigating disease progression.
Managing Diabetic Kidney Disease
Overall, CKD in diabetic patients follows a more aggressive course, and has more guarded prognosis than in nondiabetic patients. The interventions listed under CKD – lifestyle, RAAS blockade, SGLT-2 inhibitors, GLP-1 receptor agonists, mineralocorticoid receptor antagonists, and lipid lowering agents – are all effective in diabetic kidney disease, and generally have a more pronounced beneficial treatment effect than in nondiabetic CKD.
As discussed above, given the overall more guarded prognosis and greater risk of progression in diabetic kidney disease, you and your NNI provider are more likely to choose a more aggressive treatment strategy.
Vascular Diseases of the Kidney
Just as atherosclerotic vascular disease can affect the blood supply to the heart and brain, where it can cause clinical syndromes such as heart attacks and strokes, atherosclerotic vascular disease can also affect the kidneys. It can do this by causing blockages to the large and small arteries which supply blood to the kidneys. Additionally, essential or primary hypertension, when left untreated for prolonged periods of time causes damage to small vessels within the kidney called arterioles. This leads to further damage to other vital components of the kidney.
Some other less common causes of CKD are classified as being of vascular origin, diseases such as immune vasculitis, thrombotic microangiopathies, and systemic sclerosis. Our team has a great deal of experience in these areas and is quite comfortable treating these disease processes.
Managing Vascular Diseases of the Kidney
As with other etiologies of CKD, some specific vascular diseases of the kidney will require specific treatments. In the case of atherosclerotic vascular disease, some cases may be amenable to percutaneous revascularization. In other cases, optimal management may be medical therapy, including antihypertensive medications, lipid lowering drugs, and antiplatelet agents.
Primary Glomerular Disease
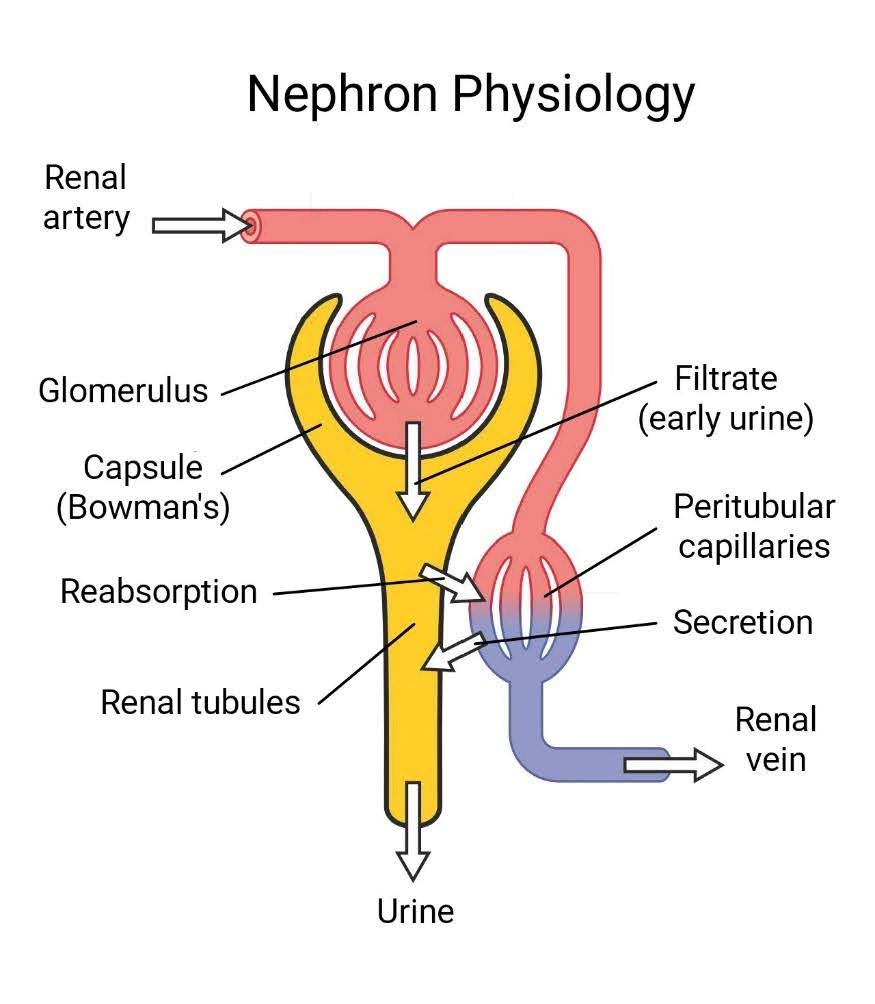
As a brief background, each kidney is comprised of roughly a million units called nephrons. Each nephron is composed of 2 main parts – a filtering unit, or glomerulus and capsule, where urine is first formed; followed by a purification and refinement system, or the renal tubules, which release urine in its final state (see image below).
In general terms, primary glomerular diseases are non-systemic autoimmune processes which affect the glomeruli of the kidney. Autoimmune diseases involve misdirection of the immune system, leading to damage of otherwise healthy tissue, in this case glomeruli.
While some diagnostic information can be obtained from blood tests, the actual diagnosis of a particular primary glomerular disease is most often made by microscopic analysis of kidney tissue obtained via image-guided renal biopsy. In fact, the various types of primary glomerular disease are classified primarily by microscopic features on renal biopsy.
Below are some more common primary glomerular diseases, listed roughly in their order of occurrence in adults:
- Focal Segmental Glomerulosclerosis (FSGS)
- Membranous Nephropathy (MN)
- IgA Nephropathy (IgAN)
- Minimal Change Disease (MCD)
- Membranoproliferative Glomerulonephritis (MPGN)
Managing Primary Glomerular Diseases
Treatment usually involves the use of immunomodulatory drugs, with the goal of taming the immune system and mitigating any damage it may have caused to the kidneys. As always, immunomodulatory drugs must be used with caution, to avoid the suppression of the immune system’s primary function, which is to protect against severe infection and malignancy.
As always, Northlake Nephrology providers are experienced and comfortable in treating these complex conditions.
Other Causes of CKD
Just as some autoimmune diseases can affect primarily the kidney, other autoimmune diseases can affect multiple systems or organs, including the kidney. These systemic autoimmune diseases include systemic lupus erythematosus (SLE) and ANCA-positive-associated diseases such as Wegener’s granulomatosis.
Some malignancies and malignancy-associated diseases can also affect the kidney and cause CKD. These include multiple myeloma (MM) and amyloidosis.
Lastly, diseases with a genetic basis may also cause CKD. These include polycystic kidney disease (PKD), Alport’s syndrome (hereditary nephritis), and Fabry’s disease.
Managing Other Causes of CKD
In many cases, treatment for these other disease processes causing CKD involves treatment of the underlying disease, including immunomodulation for autoimmune processes, as well as treatment for underlying malignant processes. In the case of genetic diseases, there are often treatments which can mitigate the underlying genetic defect.




