Advanced kidney disease occurs when declining kidney function starts to compromise day-to-day health, and without some form of renal replacement, long-term health is no longer sustainable. The term advanced kidney disease is used in lieu of the terms end-stage kidney/renal disease (ESKD/ESRD). Any distinction would be one of degree and severity, with the “end-stage” terms representing the more severe end of the advanced kidney disease spectrum.
Once advanced kidney disease has developed, there are two broad treatment approaches, one is some form of renal replacement, and the other is conservative management. In consultation with their family and healthcare providers, this is a decision that faces every advanced kidney disease patient.
Conservative Management
Advanced kidney disease often develops in conjunction with multi-organ compromise. As age, comorbidity, and frailty increase, the survival benefit offered by renal replacement decreases and eventually disappears. In many older, sicker patients the only renal replacement option available to them is in-center hemodialysis, which can have an extremely negative impact on quality of life in this patient group. These patients are often better served with conservative management.
Conservative management focuses on control of symptoms, quality of life, and preservation of remaining kidney function. Control of blood pressure, volume status, anemia, and bone health continue as with earlier stages of kidney disease, with continued use of appropriate medications and diet. Additionally, medications are used to treat other symptoms which may arise such as nausea and pruritus.
Renal Replacement
There are three major forms of renal replacement – kidney transplantation, peritoneal dialysis, and hemodialysis. Of these, kidney transplantation offers the best survival and quality of life.
Eligibility for kidney transplantation is more restrictive than other forms of renal replacement, and certain patients may not qualify due to their age and comorbidities.
Peritoneal Dialysis vs Hemodialysis
Comparing peritoneal dialysis with hemodialysis, peritoneal dialysis generally offers a higher quality of life for most patients. Survival data for the two modalities are generally similar.
The image below shows a graphical representation of peritoneal dialysis and hemodialysis, the two procedures used for chronic maintenance therapy.
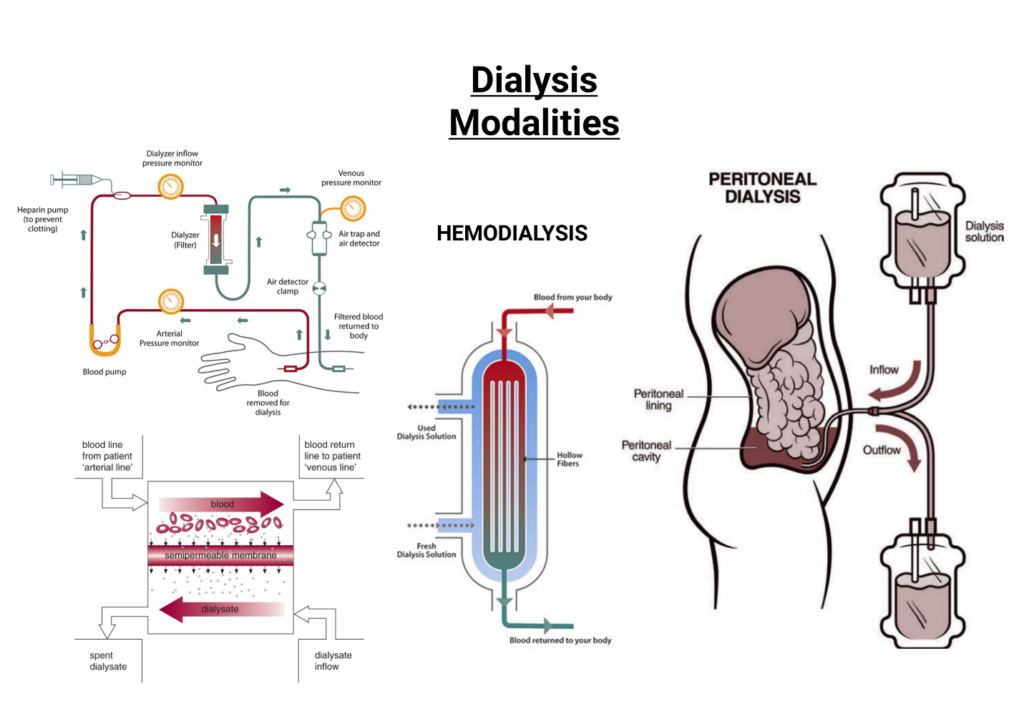
In hemodialysis, blood is removed from the body via a vascular access, pumped through an extracorporeal circuit, and returned to the body via the access. Along its course through the extracorporeal circuit, the blood passes through a dialyzer, comprised of roughly 10,000 hollow fibers composed of a semipermeable membrane. Outside of these fibers, a dialysate solution is flowing in the opposite direction to the blood. Primarily through diffusion across the semipermeable membrane, toxins are removed from the blood.
In peritoneal dialysis, dialysate repeatedly flows in and out of the peritoneal cavity via a catheter. In this case, the peritoneal membrane itself acts as the semipermeable membrane, with toxins diffusing into the dialysate which is subsequently drained out and later replaced with fresh dialysate.
Kidney Transplantation
As stated above, kidney transplantation offers a survival benefit over dialysis therapies, with matched patients on dialysis having roughly four times the mortality risk of transplant patients. Transplant patients can expect to get back 60 to 80% of normal renal function post-transplant. This is compared to 10 to 15% at best with dialysis therapy. This difference in clearance means a transplant patient with a well-functioning graft will be able to follow a diet with few if any restrictions. A liberal diet, along with freedom from the time constraints involved in dialysis, greatly enhances their quality of life.



